What anti-fraud measures could the Minnesota Legislature consider next session?
The Minnesota Legislature returns for the 2026 session next month and fighting fraud in public programs will likely be among the policies lawmakers consider.
Last year, the Legislature in bipartisan fashion approved a new anti-kickback law making it illegal for providers to make payments to individuals for patient referrals, which federal prosecutors have cited as a fixture of some of the high-profile fraud schemes.
They also authorized state agencies to withhold payments to providers suspected of fraud and increased protections for whistleblowers raising alarm of wrongdoing.
A new state House committee focused on fraud prevention and oversight met once again Tuesday where some possible ideas for session emerged. The GOP-led panel has had more than a dozen hearings since its inception last year, largely focused on the testimony of state agency leaders tasked with overseeing social services targeted by fraudsters.
Officials in Minnesota Management and Budget—which oversees the state's finances, payroll, human resources and internal controls at state departments—suggested enhancing that new law allowing agencies to withhold payments and making it permanent.
Right now the provisions sunset, she said.
"Lower the evidentiary threshold for when we can withhold payments and to allow payment withholdings to entities if fraud is discovered in one program and they are a participant in another," said Britta Reitan, deputy commissioner at MMB.
Republicans pledge to revive a bill to establish an independent Office of Inspector General, which cleared the Senate last year with broad bipartisan support. But didn't pass the House before they adjourned for the year.
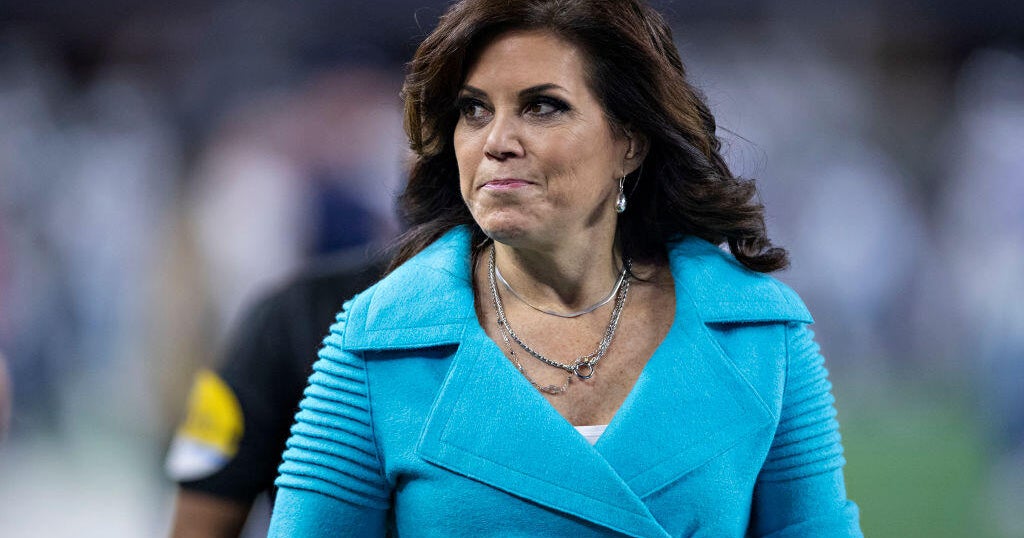
"Hopefully, after a year of uncovering all this fraud, they realize that we need that independent, independent authority. That's the key," said Rep. Kristin Robbins, R-Maple Grove, chair of the House Fraud Prevent and State Agency Oversight committee.
She also said she wants to look at changes to a law that requires health insurance companies to offer contracts to "essential community providers," which serve high-risk individuals with special needs, even if there is suspicion that those providers could be committing fraud.
DFL Rep. Emma Greenman said she hopes her colleagues will evaluate the role of private companies assisting with administration of certain state programs, like managed care organizations providing Medicaid benefits.
"We have been talking about getting private providers out of our Minnesota Health Plans for years. This year, we need to do it, because we have seen what happens when you have an incentive structure that puts profit and puts personal gain," Greenman told reporters. "We have also seen it is just very hard to have that kind of oversight"
Former top prosecutors leading the fraud investigations before their abrupt resignations earlier this month suggested the total fraud across state programs could be upwards of $9 billion. State officials dispute that figure.
One of the largest schemes involves a federal nutrition program during the pandemic. Dozens of people associated with Feeding Our Future, which oversaw several distribution sites that prosecutors say billed for fake meals, have been charged or convicted of stealing millions of taxpayer dollars.
Greenman believes that fraud underscores why there should be more scrutiny of private organizations providing taxpayer-funded services.
"We didn't see fraud in the food aid that was delivered through our public schools. We saw it in a program, in the Feeding Our Future program, which was an outsourced oversight of a federal program," she said. "So we should be looking at the structures that are accountable, that are transparent, that are publicly provided."
The Legislature convenes for the 2026 session on February 17. Any anti-fraud proposal will need bipartisan support in a politically divided capitol.