Minnesota to reevaluate nearly 6,000 Medicaid service providers to combat fraud
The Minnesota Department of Human services says it is mobilizing 168 employees from other state agencies to examine and conduct site reviews as a way to combat Medicaid fraud.
The goal is to revalidate nearly 6,000 providers across 13 Medicaid-related services by the summer, the department says. The dozens of additional staff members will review paperwork and billing, and then go on an unannounced site check.
In December, prosecutors said 14 Medicaid services that were under audit and deemed "high risk" for fraud cost the state billions of dollars. The human services department shut down the housing stabilization services program last fall.
Last year, the Centers for Medicare and Medicaid Services gave the state 26 days to come up with a plan to combat fraud. The plan was ultimately rejected; the Department of Human Services says the denial was based on reports from 2019 and 2021 and ignored corrective work that the state had shouldered over the last year.
The Trump administration has cited fraud prevention as the impetus for Operation Metro Surge.
In January, the administration said it would pull $2 billion in annual Medicaid funding from Minnesota, a decision that the state agency is appealing.
The reviews and site checks are part of an effort to convince the Centers for Medicare and Medicaid Services to backtrack on the withholding of funds. Federal data released late last month shows the improper payments of Minnesota's Medicaid program is 2.1%, far below the national average of 6.1%.
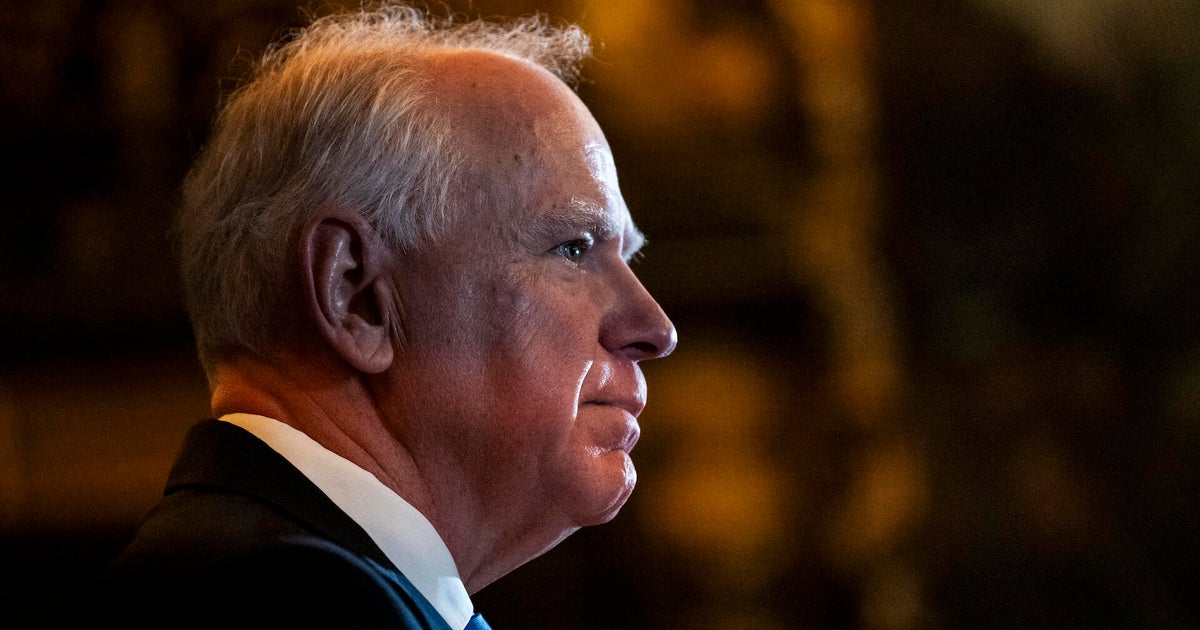
"We're implementing their recommendations, and we are taking action above and beyond those requests to minimize the risk of fraud, harden our systems against bad actors, and catch fraud quickly when it does happen," said John Connelly, deputy commissioner and state Medicaid director.
Providers across all 87 Minnesota counties will be assessed.