A mom-to-be started screaming in pain on her babymoon. Here's how doctors saved her and her baby.
Cassandra King was thrilled to complete the first trimester of her pregnancy in the fall of 2024. She and her husband had spent years trying to have a baby, and she had experienced multiple miscarriages. The couple decided to celebrate with a babymoon to Jamaica during the 17th week of her pregnancy.
At first, the trip went smoothly. King only felt "a little bit of pregnancy discomfort." Then came the "burning, spasming pain" in her shoulder on their final night. It felt like a fist between her shoulder blades and down her spine, King said. She vomited for two hours before going to a local hospital, terrified and "screaming" in pain.
"I remember pleading with the tech, 'Please, please tell me if my baby is still alive,'" King said. "I was fairly early in my pregnancy. I hadn't felt her kick yet. I knew something was wrong, but not the extent of what had happened. Did my body go into survival mode? Did she not get enough oxygen? I didn't know."
Doctors found that King had experienced a spontaneous coronary artery dissection — a sudden cardiac event caused by a tear in an artery. The next day, King was medically evacuated to Atrium Health Wake Forest Baptist Hospital in North Carolina.
The situation was critical. King's heart was failing. The average heart pumps out between 55% and 60% of its volume with every heartbeat, according to Dr. Bartlomiej Imielski, a cardiothoracic surgeon who was one of the lead doctors on King's case. King's heart was only pumping out about 25% of its volume. Her pregnancy was putting even more strain on her body. Doctors recommended she terminate her pregnancy — something King couldn't consider.
"I had a sense of peace. I knew, in my heart of hearts, without the shadow of a doubt, that I was going to survive this. I realized I couldn't live with myself knowing I had voluntarily terminated my daughter's life. I would always feel selfish. I would always wonder," King said. "I put three years of, literally, blood, sweat and tears into this. ... But of course, then came a very hard question: What do we do?"
"Constantly weighing risks and benefits"
Multiple teams worked on King's case to develop a path forward that everyone was comfortable with, Imielski said.
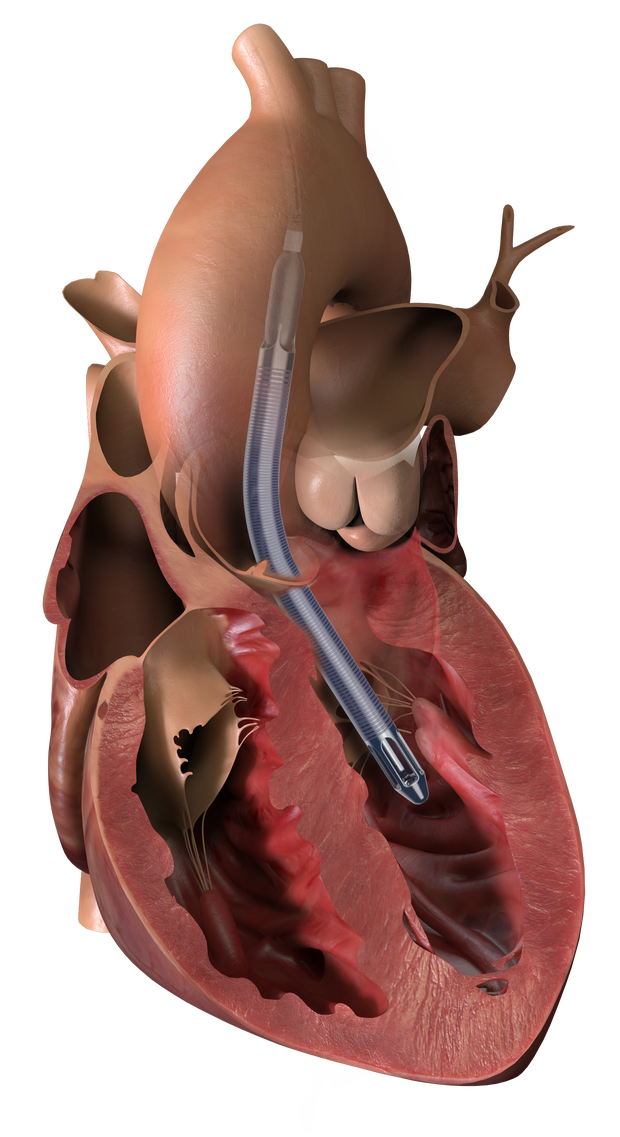
For as long as possible, they would support King and her baby with medication. When those no longer worked, they would use a device called the Impella 5.5 to help her heart pump blood. The medical team hoped to get King's pregnancy to at least 24 weeks, when fetuses are generally considered viable outside the womb.
The Impella 5.5 had previously only been used in pregnancy-related cases about half a dozen times, Imielski said. All of those cases had been mothers who were either about to deliver or in the postpartum period. It had never been used to help a patient from the non-viable stage of pregnancy get to the point where a baby could be successfully delivered.
"You felt the consequences. You had a mother's life on your shoulder, a baby's life on your shoulder, and you were doing something that you could very easily get criticized for, because there was no 'This is how we do it,'" Imielski said. "It was very clear we were kind of creating the path here. ... We were constantly weighing risks and benefits."
"You've done everything you can"
King had weekly check-ins through the holiday season. On New Year's Eve, King began experiencing chest pain, swelling and shortness of breath, and went back to the hospital. Tests showed her heart needed the support of the pump, so she was taken into surgery. There were over 20 medical professionals gathered in the operating room, Imielski said.
Just minutes into the procedure, King's blood pressure dropped. Her baby began to show signs of distress.
"Maternal-fetal medicine and the neonatologist basically said 'The fetus is not doing well. You have 10 minutes to do this, or we're going to have to do a crash C-section,'" Imielski said. Doctors wound up briefly putting King on life support to safely complete the procedure.
King spent the next 13 days in the ICU as the Impella 5.5 kept her heart functioning. On January 13, she was told that tests were showing worrying fetal activity. If King or her baby became unstable, the maternal-fetal medicine team was worried one or both of them might not survive an emergency delivery. With King 27 and a half weeks into her pregnancy, the neonatal specialists felt the baby had a 95% chance of survival without deficits, Imielski said.
"They said 'You've done everything you can for this baby,'" King said. "So I agreed."
"Perfect in every way"
King's C-section took place in another crowded operating room, with her medical team prepared for every outcome. Her daughter, named Persephone, was born weighing just two pounds, four ounces. She was small enough to fit in her father's hand, but she was doing well and breathing on her own.
"Knowing that I had gotten her there, that I was going to get to meet her, I was going to get to raise her, that we got there, was profound. There were no words to describe what that felt like," King said. "She was perfect in every way."
Three days later, King's heart pump was removed. Five days after that, she was released from the hospital. Persephone spent three months in the NICU and was released in March. King had six stents implanted in May, completed a cardiac rehabilitation program in November and continues to have regular check-ups. Persephone is now a happy, healthy 1-year-old, King said.
"It's been everything to me to get to be a mom to her," King said. "She is so sweet. She's just absolutely wonderful."
King said she hopes her experience will change care for others. Imielski said the procedure likely won't be standard care any time soon, but that King's case "opens up a frontier for research and investigation."
"We've proven that if a family, if a mother chooses to go against recommendations, we could consider a plan B," Imielski said. "It's still something that is in its infancy, that needs to be done more, that needs to be researched more, but I'm excited that we have a plan B."