Shortage of nursing home staff fueled COVID-19 outbreaks, consumer group says
The nursing home industry's long-standing staffing problem was made even worse by the pandemic, and consequently may have contributed to its struggle to keep residents safe from COVID-19, according to a recent report.
More than 3,000 nursing homes in the U.S. — roughy a fifth of facilities — were understaffed during the month of December, U.S. Public Interest Research Group said in a report. These long-term care facilities experienced shortages of nursing aides, doctors and other health care staff with direct patient contact at a time when they were needed most, the consumer watchdog found.
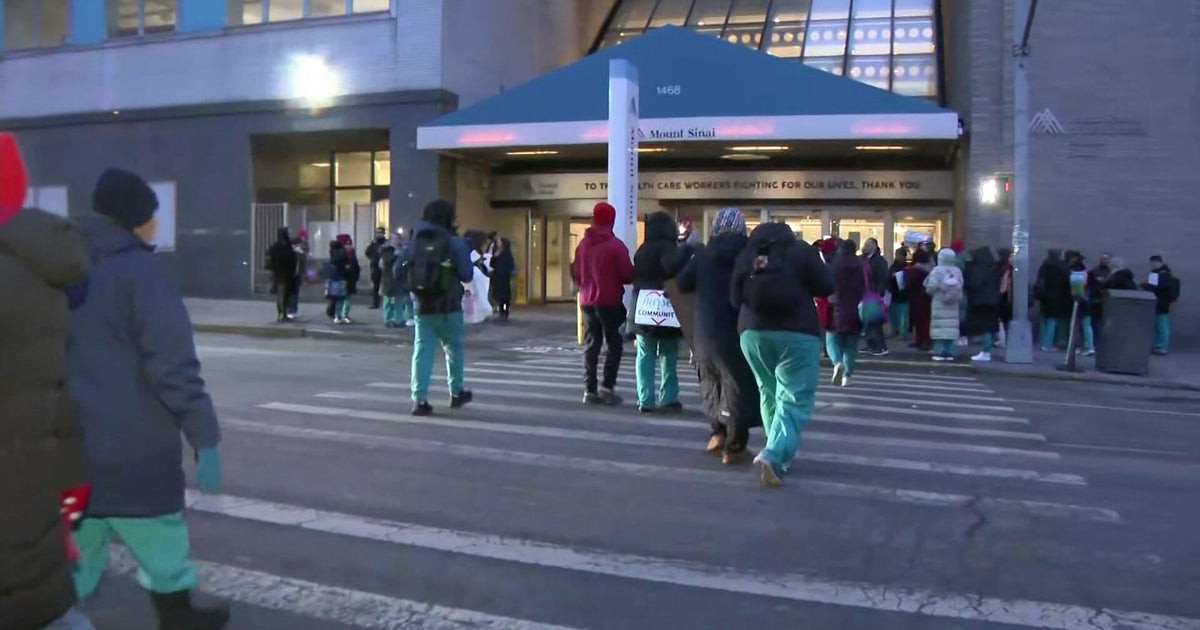
Nursing home workers have notoriously taxing jobs, while pay is low. Many nursing home workers, already stretched thin, contracted COVID-19 themselves, forcing them to leave the facilities and self-isolate for a period of time. These absences fueled more outbreaks, as remaining staff members interacted with greater numbers of residents at once.
Nurse shortage affected 18.5% of all nursing homes in December, US PIRG found. Higher staffing levels, in contrast, were found to prevent deaths. Nursing home residents represent about 1% of the the U.S. population but have accounted for 2% of all COVID-19 infections, and 25% of deaths from the virus.
"Not only are the shortages a direct result of the COVID-19 pandemic, experts say, but in a circular nightmare, the staff shortages also fueled more COVID outbreaks in nursing homes among residents and staff," US PIRG said in the report.
Not enough PPE
Another hurdle plaguing many nursing homes during the pandemic has been insufficient supplies of personal protective equipment, which is widely regarded as instrumental in warding off infection. A separate U.S. PIRG report found that in December, 8% of nursing homes across the U.S. did not have enough surgical-grade N95 masks.
"This is indefensible. Nursing home workers desperately need these supplies to take care of themselves, their patients and the broader community," US PIRG staffer Teresa Murray said in a statement.
PPE supply levels improved during the fall, but worsened again in December as demand spiked, in part because health care workers administering the vaccine are required to wear masks and other protective gear.
Although worker turnover in the nursing home industry has always been high, the pandemic has worsened the problem. Some clinical care staffers, overwhelmed by the stress and fear of catching COVID-19, have left the field altogether.
Still, other nursing home professionals, many of them women with young children, were forced to quit their jobs to stay home to help their kids with remote schooling. Other skilled workers also found themselves taking time off to care for loved ones at home who had contracted the virus, according to the report.
The consumer watchdog group believes more emergency COVID-19 funding should be directed to nursing homes to enable them to hire more staff and compensate workers with higher wages and bonuses.
The director of a nursing home in Baltimore, Maryland, said he hired additional staff members and also upped workers' pay to help retain staff and ward off the virus. That approach proved successful — the facility has had zero cases of COVID-19, the director, Rev. Dr. Derrick DeWitt, recently told CBS MoneyWatch.
A federal initiative to boost PPE production and COVID-19 testing would also go a long way, according to the U.S. PIRG report.