Breakthrough Status
Editor's Note: For more information on the Duke University polio trial or other brain cancer trials, click here or call the Preston Robert Tisch Brain Tumor Center at Duke 919-684-5301
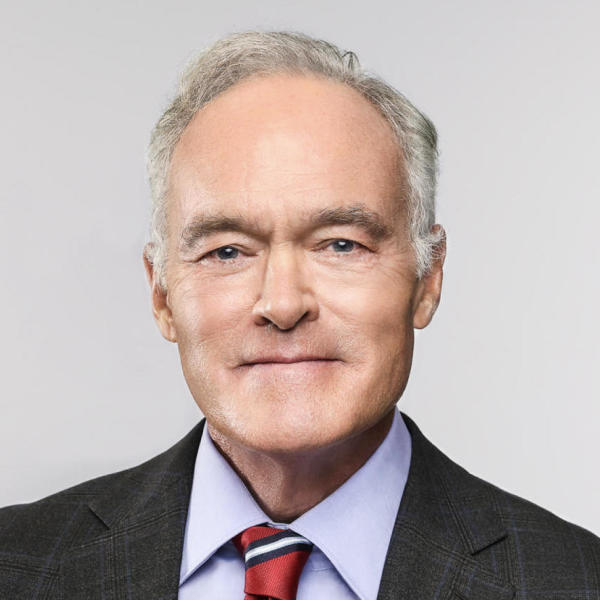
The following is a script from "Breakthrough Status" which aired on May 15, 2016. Scott Pelley is the correspondent. Denise Schrier Cetta and Michael Radutzky, producers.
A bold experiment to kill a vicious cancer has won breakthrough status from the Food and Drug Administration. Early tests at Duke University have been so successful the FDA will fast track this treatment to hundreds of patients while it's still being evaluated for final approval. The therapy is audacious. It uses the polio virus to attack a virulent brain cancer called glioblastoma - which is a death sentence of astonishing speed that leaves patients with only months to live. For two years, we've been following volunteers in the Duke clinical trial. We have witnessed nearly miraculous recoveries and unexpected defeats on a journey of discovery beyond the known frontiers of science.
Nancy Justice had been sentenced to a bleak prognosis when we met her in October 2014. At age 58, she had recurrent glioblastoma. It had come back after surgery, radiation and chemotherapy. Typically, she could expect to live seven months. The polio virus which mankind had fought to eradicate from the Earth, was the last chance she had in the world.
Nurse: ...feel a tiny tug there...
A half a teaspoon of polio flowed through a catheter inserted through Nancy's skull, directly into her tumor.
Nurse: OK. Ready to go?
Nancy Justice: I'm ready, bring it on.
Nurse: We're starting.
Dr. Annick Desjardins: If you feel anything, you let us know.
Nancy Justice: I will, definitely.
Her husband, Greg, constantly inflated a buoyant optimism to save him from the weight of the unknown. Her glioblastoma was diagnosed in the 21st year of Nancy and Greg's marriage -- just as the Georgia couple could make out the finish line for Zach and Luke at college. Her tumor can double in size every two weeks.
Scott Pelley: The tumor was aggressive--
Nancy Justice: Yes.
Scott Pelley: So you wanted an aggressive treatment--
Nancy Justice: Yes. Yes.
Scott Pelley: You're a medical explorer. Does it feel that way to you?
Nancy Justice: I'm taking it one day at a time. It sounds very lofty to say medical explorer. But you know throughout all of this if this gives other people hope I'm all for it.
Scott Pelley: Greg, you mentioned that Nancy was there for every important event in the boys' lives.
Greg Justice: Right.
Scott Pelley: But, there a lot of important events to come.
Nancy Justice: Exactly.
Scott Pelley: What do you hope to see?
Nancy Justice: So I am gonna see those boys walk across the stage at their college graduation. I am gonna see 'em get married. And I am gonna see the grandkids, preferably in that order. And I know it's, like, such a mom bucket list. But I'll love every minute of it.
This is Duke's polio team, Dr. Darell Bigner, director of the Tisch Brain Tumor Center, molecular biologist Matthias Gromeier and neuro-oncologists Dr. Henry Friedman and Dr. Annick Desjardins. As is typical, the university has licensed this technology to a new company to attract research dollars to the therapy and all the members of the team are investors.
Dr. Henry Friedman: Good to see that this is going well.
Dr. Friedman screens more than 1,000 glioblastoma patients a year who would like to be treated at Duke. He helps decide who meets the criteria for the polio trial.
Scott Pelley: I wonder of all the trials and all of the theories and all of the treatments that you have hoped for all of these years, how does this stack up?
Dr. Henry Friedman: This, to me, is the most promising therapy I've seen in my career, period.
The virus is the creation of, the obsession of Dr. Gromeier, who has been laboring over this for more than 25 years, the last 15 at Duke.
Scott Pelley: When you went to your colleagues and said, "I've got it. We'll use the polio virus to kill cancer." What did they say?
Dr. Matthias Gromeier: Well, I got a range of responses from, from crazy to you're lying, to all kinds of things. Most people just thought it was too dangerous.
Dr. Henry Friedman: I thought he was nuts. I mean I really thought that what he was using is a weapon that produces paralysis.
Other researchers are experimenting with cancer treatments using viruses including HIV, smallpox, and measles.
But polio was Dr. Gromeier's choice because, as luck would have it, it seeks out and attaches to a receptor that is found on the surface of the cells that make up nearly every kind of solid tumor. It's almost as if polio had evolved for the purpose.
Gromeier re-engineered the virus, removing a key genetic sequence. The virus can't survive this way so he repaired the damage with a harmless bit of cold virus. This new modified poliovirus can't cause paralysis or death because it can't reproduce in normal cells. But in cancer cells it does and in the process of replicating it releases toxins that poison the cell. At least that's what they'd observed in the laboratory. Eventually they had to try it in a human being.
It's a hell of a thing to be told that you have months to live when you're 20 years old. In 2011, Stephanie Lipscomb was a nursing student with headaches. A doctor told her she had this glioblastoma tumor the size of a tennis ball.
Stephanie Lipscomb: I looked at the nurse that was sitting there holding my hand and-- I said, "I don't understand. Like, what did he just say?" It was kind of hard for me to process.
Scott Pelley: You had 98 percent of the tumor removed.
Stephanie Lipscomb: Exactly.
Scott Pelley: As much radiation as you can have in a lifetime. And chemotherapy.
Stephanie Lipscomb: Exactly.
Scott Pelley: And then in 2012, what did the doctors tell you?
Stephanie Lipscomb: Your cancer's back.
With recurrent glioblastoma, there were no options except the one that had never been tried.
Scott Pelley: Did they tell you that it had never been tried in a human being before?
Stephanie Lipscomb: They did. But at the same time, I had nothing to lose, honestly.
Her polio treatment began in 2012 and from the very beginning it looked like a bad bet.
Dr. Annick Desjardins: So we treated her in May. Then in July the tumor looked bigger, looked really inflamed. I got really concerned, got really worried.
Scott Pelley: You thought this wasn't working.
Dr. Annick Desjardins: I thought it wasn't working.
Neuro-oncologist Annick Desjardins wanted to abandon the polio experiment and return to traditional treatment. But Stephanie said "No." Five months after her infusion, an MRI showed the tumor only looked worse because of inflammation caused by Stephanie's immune system which had awakened to the cancer for the first time and gone to war.
Scott Pelley: Why didn't the immune system react to the cancer to begin with?
Dr. Matthias Gromeier: So cancers-- all human cancers, they develop a shield or shroud of protective measures that-- make them invisible to the immune system. And this is precisely what we try to reverse with our virus. So by infecting the tumor, we are actually removing this protective shield. And telling the, enabling the immune system to come in and attack.
Scott Pelley: So essentially what's happening here inside the tumor is you have a polio infection.
Dr. Matthias Gromeier: Yes.
Scott Pelley: And that sets off an alarm.
Dr. Matthias Gromeier: Yes.
Scott Pelley: For the immune system.
Dr. Matthias Gromeier: Yes
Scott Pelley: The immune system says, "There's a polio infection. We better go kill it."
Dr. Matthias Gromeier: Exactly.
Scott Pelley: And it turns out it's the tumor.
Dr. Matthias Gromeier: Yes.
It appears the polio starts the killing but the immune system does most of the damage. Stephanie's tumor shrank for 21 months until it was gone. Three years after the infusion something unimaginable had happened. This is from an MRI in August 2014.
Scott Pelley: And there's no cancer in this picture at all--
Dr. Annick Desjardins: And we don't see any cancer, active cancer cells.
She is cancer-free. All that remains is this hole from an early surgery.
Scott Pelley: How surprised are you by that?
Dr. Henry Friedman: I'm surprised because you never expect on a Phase 1 study in particular to have these kinds of results.
Scott Pelley: You're not expecting to cure people in a Phase 1 trial.
Dr. Henry Friedman: You're not even necessarily expecting to help them. You hope so. But that's not the design of a Phase 1 study. It's designed to get the right dose. When you get anything on top of that it's cake.
Scott Pelley: Quite a cake.
Dr. Henry Friedman: Quite a cake. Quite a cake. Biggest cake we've seen in a long, long time.
Dr. Fritz Andersen showed us the results in another patient, himself. He's a retired cardiologist and at age 70, he became the second person in the polio trial.
Dr. Fritz Andersen: This is a fairly sizeable temporal tumor, which means...
Scott Pelley: That we see right here.
On the left is his tumor before treatment, on the right a hairline scar where it used to be. That was nearly three years ago.
Scott Pelley: Do you consider yourself cured? Or do you call it remission?
Dr. Fritz Andersen: I feel it is a cure, and I live my life that way.
After the early successes, the next patients would receive a higher dose. That's the whole idea behind a Phase 1 trial--to increase the dose in succeeding patients, step-by-step, in search of the highest dose that is still safe.
Dr. Henry Friedman: We believe in the philosophy we've learned in chemotherapy that more is better. So if we were getting a good response at dose level one or dose level two, then go to dose level three, four, five.
Sixty-year-old Donna Clegg was a social worker from Idaho. We met her in 2014, puffy from the steroids used to reduce the swelling in her brain.
Donna Clegg: I wanna be able to live. So that's kinda how I feel, that this is gonna be my opportunity to have a full life.
Donna's polio infusion was three times more potent than the one that had worked for Stephanie. But in her case this higher dose set off an immune response that was much too powerful. Donna battled the inflammation for nine months, before she died in March 2015.
Scott Pelley: Donna Clegg suffered quite a lot. And I wonder how that weighs on your mind?
Dr. Henry Friedman: Every patient who has an outcome that is not positive weighs on my mind. I think that when you're doing a Phase 1 study, you know that these things can happen. But she is a patient who really did not derive benefit and yet taught us something important.
Scott Pelley: You discovered that putting in too much poliovirus created too large an immune response?
Dr. Henry Friedman: Absolutely.
After that hard lesson, doctors cut the potency of Nancy Justice's dose by 85 percent. It was less than they had ever expected to use. They called this new dose, "Dose Minus 1." But even so, four and a half months after her infusion, in March 2015, inflammation had caused the mass in Nancy's brain to double in size. But to Dr. Desjardins the tumor looked weaker.
Scott Pelley: And in this image, it's shot through full of holes.
Dr. Annick Desjardins: It's shot through full of holes. And let me show you the next picture and you'll see it's even--
Greg Justice: Wow.
Dr. Annick Desjardins: --more and more holes.
Scott Pelley: So where does this go from here?
Dr. Annick Desjardins: So now, we keep following her. And hopefully it keeps shrinking and it keeps collapsing. And that's what we have seen with Fritz and Stephanie, that it continued shrinking for years.
Scott Pelley: Nancy, when you look at this, what do you think?
Nancy Justice: Oh, it's amazing. Oh my gosh. I'm mean, thank you lord. And these doctors. Thank you doctors. You know, and to just see this, um, you know, that's life.
Nancy Justice faces a hard road ahead, but along the way new discoveries will take the researchers in a direction they never imagined.
Part Two
Thirty-eight patients have volunteered for Duke University's experiment to use the poliovirus to kill glioblastoma, the most efficient, relentless cancer of the brain. The FDA's decision to grant Duke "breakthrough status" means the second phase of the trial will be expanded to about 40 institutions with hundreds of patients. If that goes well, Duke will be allowed to skip the third phase of the trial and make polio therapy for glioblastoma available to all.
The route to this achievement was not a straight line. The first volunteers saw their tumors disappear. But later patients suffered crippling setbacks. There was a way forward but researchers found themselves on a path they had not imagined. Their guide through the mystery was a patient named Brendan Steele.
On Christmas Eve, 2009, Brendan Steele could not know how precious the gift of life would be. At 37, he was an IT manager in Montana, a husband and father of three. But then doctors found glioblastoma and gave him 11 months to say goodbye. When surgery, radiation and chemotherapy failed, Brendan volunteered for Duke's polio trial and in 2013 he received the six-hour poliovirus infusion. But in removing the catheter a blood vessel was severed. His wife Kathy was by his side.
Kathy Steele: Brendan said, "It's weird." And he goes to hold his head and "weird" just kinda drained out. Like, that was the end of his speech.
Scott Pelley: You understood how bad off you were?
Brendan Steele: No.
Scott Pelley: No?
Brendan Steele: No, because I don't remember.
Emergency surgery stopped the bleeding, but the trauma left Brendan barely able to walk or talk. Seven months later a biopsy revealed that his tumor was growing. Doctors gave Brendan chemotherapy. It had failed him before, but it might give him just a few more weeks. Neuro-oncologist Annick Desjardins did not imagine what happened next.
Dr. Annick Desjardins: We gave him one dose of chemotherapy. And the lesion just melted. Went away. Rapidly. Which we don't see that happen normally.
Two months after that single dose of chemo, the tumor -- the white mass on the right -- started to break up. Brendan continued the chemotherapy and in eight months, it was gone.
Scott Pelley: And what did the doctors tell you about your cancer today?
Brendan Steele: No cancer. No cancer.
Scott Pelley: Recurrent glioblastoma and now they tell you they cannot find it in your brain?
Brendan Steele: Yep.
Brendan Steele has lived 35 months since his polio infusion. He's been cancer-free for 19. Dr. Henry Friedman, deputy director of Duke's Cancer Center, has a theory about why the chemo worked this time, when it never had before.
Dr. Henry Friedman: Shockingly, chemotherapy in patients who have previously failed it, once they've had the poliovirus therapy, now seem to have a new enhanced, almost extraordinary response to the chemotherapy as if the poliovirus has set up the tumor to be more responsive to chemotherapy.
Scott Pelley: That was a surprise?
Dr. Henry Friedman: That was a surprise. And for us to see this, it was a stunning observation, that is actually the platform for a future study that will involve chemotherapy and the poliovirus.
The discovery changed their approach to Nancy Justice. You'll remember when we last saw Nancy in March 2015, Dr. Desjardins saw signs her tumor was breaking up. But, in the months that followed, the inflammation kept growing. As Nancy's brain compressed, she was losing the connection to her arm...her legs...and her relationship to the very space around her.
Nurse: And touch your nose. Here...
Nancy Justice: Like this?
Nurse: Yep. Touch your nose.
Whatever part of the brain involves the will to fight, appeared to be unaffected. Now, would a single dose of chemo have the same miraculous result as it did for Brendan Steele? Dr. Desjardins reached for their new discovery and within two months, the mass was shrinking.
Dr. Annick Desjardins: See how the folds of the brain are back when they were all squished up?
Nancy Justice: Oh wow.
Dr. Annick Desjardins: The ventricle is reopening.
Greg Justice: Look at that. Hallelujah! Now, that's what we're looking for honey!
Scott Pelley: How did you feel at that time?
Nancy Justice: Oh. Loved it. Love, I mean, that's what we'd been working for, praying for.
Scott Pelley: Tumor's getting smaller and smaller and less...
Greg Justice: Somebody had taken an eraser to it.
As the inflammation retreated there was new space for hope.
Physical therapist: Up, up, up, up, up. Elbows straight. Elbows straight.
Greg Justice: Look at the speed, honey.
Nancy found strength and, buoyed, always, by her husband Greg, she walked up to a mile a day. Nancy's life was covering a distance of time denied to glioblastoma patients, but last February, 15 months after her infusion of polio, her run met another hurdle.
Dr. Annick Desjardins: Just a little more inflammation.
The day her journey began she told us she would see her sons graduate, be married and have children, in that order, she joked, now determination was nuanced with gratitude for what she'd had already.
Scott Pelley: Nancy, when we met you the first time, I asked you about your mom bucket list. How are those weddings and grandkids looking to you now?
Nancy Justice: OK. So, right now, I'm thinking it's just the simple things right now that I enjoy.
Seven weeks after that interview - in late March -- Nancy was rushed back to Duke. The light that never dimmed was in her eyes but her words were gone. This is what she was fighting. The inflammation engulfed half her brain.
Dr. Allan Friedman: I just think we need to know what we are dealing with so we can move.
Neurosurgeon Allan Friedman needed to find out if the mass was a buildup of dead cells from the immune response or active cancer. He slipped a needle into her brain to extract a bit of tissue.
Dr. Allan Friedman: Thank you. See you back there in a second.
The tissue was rushed to the pathology lab where a microscope discovered dead cells where the polio was working, but also regrowth of the tumor. Glioblastoma had found a way back.
Dr. Annick Desjardins at bedside: Hey Nancy, how are you doing?
Seventeen months after we first met Nancy, doctors Allan Friedman and Annick Desjardins explained to Greg that Nancy's tumor had now infiltrated parts of her brain responsible for breathing and cognition.
Dr. Annick Desjardins: She's getting worse and maybe it's the time where we cannot do anything anymore to help her. And we need to let her go.
Dr. Annick Desjardins: And we love you, you know that, right?
We wondered whether Greg would do it all again.
Greg Justice: Definitely we would do it. Nancy would've been gone long ago. And I think it's given us some good time. And we appreciate that.
On April 6th, Nancy Justice, medical explorer, passed away at the age of 60. She'd had nine more months than she could have expected.
Scott Pelley: What did Nancy teach you?
Dr. Annick Desjardins: From the treatment standpoint, what she taught us is two different things. So clearly, the combination of the poliovirus with the chemotherapy had, at first, an amazing response. We need to understand that. The next thing is, at some point though, it stopped working. And why did that happen?
What the Duke team has learned is that inflammation is an unavoidable consequence of the immune system's attack in most patients -- and that managing it with drugs will likely be a key to survival.
Scott Pelley: So far there have been 21 patients at this lowest dose, minus one.
Friedman: Yes.
Scott Pelley: Eight of them have died.
Friedman: Yes.
Scott Pelley: Put that in perspective for me.
Friedman: All the ones who haven't died, on a Phase 1 trial, is simply remarkable. And to see positive results in terms of controlling a tumor or shrinking a tumor in patients with recurrent disease on a Phase 1 trial is remarkable. It's not your goal, it's not your expectation. But it certainly is something that when you see it, you say this is really terrific. This is special.
Apparently the FDA saw something special too. Breakthrough status was granted after data showed that patients who had been living an average of 10 months were living an average of 15 months. And three patients, showed no sign of cancer at all after three years.
Dr. Darell Bigner, who runs Duke's Brain Tumor Center, has fought glioblastoma for 50 years.
Scott Pelley: When you talk of median survival being extended from 10 months to 15 months, for some of these patients, it's 15 months and counting.
Dr. Darell Bigner: Yes.
Scott Pelley: They're still living.
Dr. Darell Bigner: Yes. Yes, and we still have got significant periods of high quality survival. And that is a huge difference. And then we have patients like Stephanie, Fritz and Brendan that are leading virtually normal lives. I mean, they probably go many days without even thinking about having had a glioblastoma, which is just amazing.
Scott Pelley: You were in medical school thinking about one day being able to beat glioblastoma. And now you are standing on this doorstep. What does that mean to you personally?
Dr. Darell Bigner: It's an enormous feeling. And I have to be very careful. I never want to give anyone false hope. But I see all of the science coming together now. And I know it's gonna happen. I've never felt that way until now.
And in an amazing new development, this science may be "coming together" for an entire range of cancers. In the laboratory, Duke has used polio to kill cancer cells of the skin, pancreas, stomach, lung, colon and prostate. Immunologist Dr. Smita Nair showed us what polio did to breast cancer in mice.
Dr. Smita Nair: This is breast cancer tissue. And what we find is, if you look at this is, here is a tumor that got injected with poliovirus. Here is a tumor that got injected with just saline. And the difference in the tumor size is extremely visible here.
Scott Pelley: Night and day.
Dr. Smita Nair: We kept seeing this. So we went back and asked the question, "What is happening in the tumors?" And we teased these tumors apart. And what we found were a lot of T-cells in the tumor.
Scott Pelley: Immune system cells?
Dr. Smita Nair: Immune system cells.
Dr. Nair has filmed immune system T-cells, shown here in color, breaking apart a tumor cell. What you see took a little over one hour. This leads Dr. Nair and others to a fascinating possibility. Once immune cells are programmed to recognize a cancer, will they remember and attack that cancer everywhere in the body for a lifetime?
Dr. Smita Nair If you get a tumor again, these are memory T-cells, they will remember that. And they can eliminate a recurrent or a metastatic tumor.
Scott Pelley: How long does it take typically to get from this mouse stage into a human trial?
Dr. Smita Nair: I would say anything between three to five years. It takes some time.
Scott Pelley: Well, go back to work and stop talking to me.
Dr. Smita Nair: That's what I will do. That's what I think I should do.
Physical therapist to Brendan Steele: Remember two months ago you couldn't lift that heel.
There is much left to learn. Why do some patients suffer and die while others given months to live appear to have a complete recovery?
Three years after his polio treatment Brendan Steele remains cancer-free and he's determined to overcome the damage from his surgery, a conviction that he keeps within arm's length.
Scott Pelley: "It's not whether you get knocked down, it's whether you get up." Great words to live by.
Brendan Steele: Yeah. Yeah. I remind myself every day. Get up. Get up.
Four years after his polio therapy, 73-year-old Fritz Andersen is traveling the world with his wife.
Fritz Andersen: I'm alive because of it. If I hadn't received it I don't think I would be here today.
And Stephanie Lipscomb, Patient Number One in the clinical trial four years ago, has now become a nurse.
Stephanie Lipscomb: Do you remember me coming in this morning, I know you were sleepy?
Patient: Yes.
Scott Pelley: You told us before that being a cancer patient would probably make you a better nurse. And I wonder, has it?
Stephanie Lipscomb: Oh yes. To talk to my patients and tell them, "Look, I've been, I've been in the hospital, I've been sick like this." I can just see the hope in their eyes.
Scott Pelley: Where do you want to take your nursing career?
Stephanie Lipscomb: Pediatric oncology.
Scott Pelley: Kids with cancer.
Stephanie Lipscomb: Yes sir. Because I was 20 when I was diagnosed. I wasn't really completely an adult. And I absolutely love kids. With this unique experience of surviving Stage IV cancer in my brain. If I don't do this, then it's kinda like a waste. A waste of being cancer-free.
Scott Pelley: You think you survived for a reason?
Stephanie Lipscomb: Oh yes, most definitely.