Patients still not protected from surprise ground ambulance bills
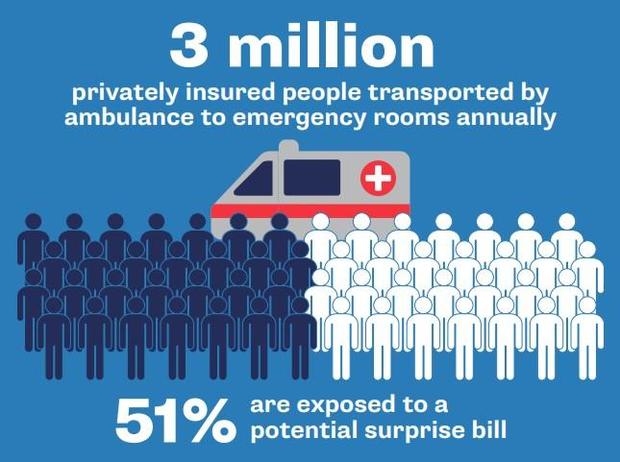
AUSTIN (CBSNewsTexas.com) – When you dial 911, chances are you are not thinking about how much the ambulance ride will cost. But when it comes to time pay, millions of insured Americans every year are blindsided with a surprise medical bill.
According to a U.S. PIRG Education Fund study, more than 50% of insured patients are at risk of receiving an out-of-network bill for an ambulance ride. In Texas, the risk is 70%.
"You expect when you have insurance, when you pay for insurance, that they will be there for you when you need it," said Rachel Carnahan-Metzger, whose 5-year-old daughter was rushed to the hospital by an ambulance after a fall.
The five-mile ambulance ride from their home in Austin to the hospital cost the Metzger family $1,082 out-of-pocket. Austin-Travis County EMS, the only emergency ambulance provider in the area, does not contract with any private insurance companies – meaning all its ambulance rides for patients with private insurance are billed out-of-network.
"It's frustrating," Metzger said. "It feels bad to feel like you are getting ripped off by these people that are supposed to be proving you lifesaving services."
Every year, out-of-network ground ambulance rides cost insured Americans $129 million, according to a 2020 study published on Health Affairs.
The 2020 No Surprises Act was supposed to do away with surprise out-of-network emergency medical bills. While the federal law has protected patients from out-of-network bills from hospitals and even air ambulance services, an exception was made for ground ambulances.
Tuesday, a federal advisory committee tasked with finding a way to eliminate surprise ambulance bills will meet virtually for the first time. The committee is made up of government officials, members of the ambulance and insurance industries, along with a consumer advocate.
The committee has six months to make recommendations to Congress. The formation of the committee was part of 2020 No Surprises Act. While lawmakers were reluctant to include ground ambulance services on surprise bill bans, they did acknowledge a better understanding of the cost of ambulance services was needed.
"We really need to solve this," said Patricia Kelmar, the U.S. PIRG senior director of health care and lone consumer advocate on the advisory committee. "It's not fair if you are insured that there's a good chance you can't even go in-network for an ambulance."
While private corporations provide some ambulance rides, most 911 emergency ambulance calls are provided by local government agencies. In Dallas, it's Dallas Fire-Rescue. In Fort Worth, it's MedStar.
Matt Zavadsky of MedStar said if local government-run ambulance services could only collect what insurers are willing to pay, either local taxes would have to go up to make up the difference or the level of service would have to go down.
"I would argue that if the community wants to have an ambulance at their heart attack, at their car crash, at their baby not breathing within seven minutes with a high degree of reliability, it costs a lot more than $500 to do that," Zavadsky said.
While ambulance services say the problem is insurers under-paying, insurers say the problem is ambulance providers' refusal to be in-network. Both sides say patients should not be stuck in the middle, but currently patients are.
An Austin-Travis County EMS spokesperson told the CBS News Texas I-Team it advises patients to contact their insurance and explain that ATCEMS is the only emergency provider in the area, and ask them to re-process the claim as in-network. The Metzger family did that but were unsuccessful at getting their insurance provider to process the claim as in-network.
After unsuccessful attempts to negotiate, the Metzger family began making monthly payments on their ambulance bill. Their daughter, June, 5, will be nearly 8 years old by the time they pay it off.
A spokesperson for Blue Cross Blue Shield of Michigan, the Metzger's insurance provided, provided the I-Team with the following statement:
"When someone has an emergency and needs an ambulance, the last thing they should have to worry about is receiving a surprise bill from an out-of-network ambulance company. Ambulance companies should work with health plans to ensure their services are in network. The current law stops short of addressing surprise billing challenges with ground ambulance services. We are supportive of extending protections for patients for these services and look forward to seeing the recommendations proposed by the NSA-required Ground Ambulance and Patient Billing Advisory Committee to address this gap."