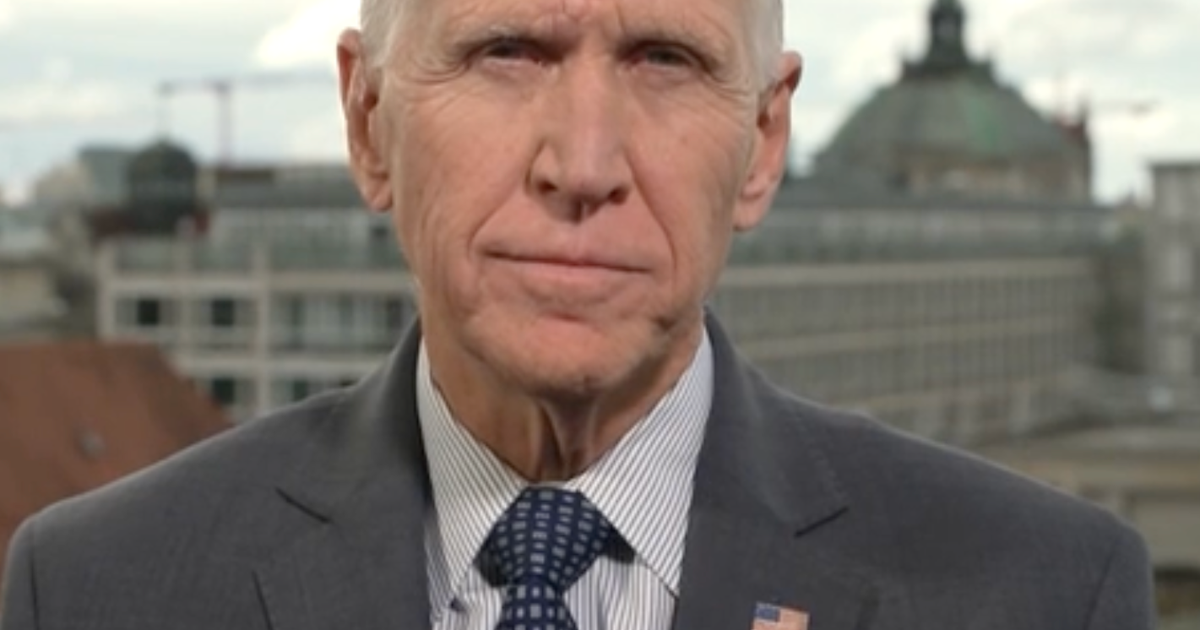
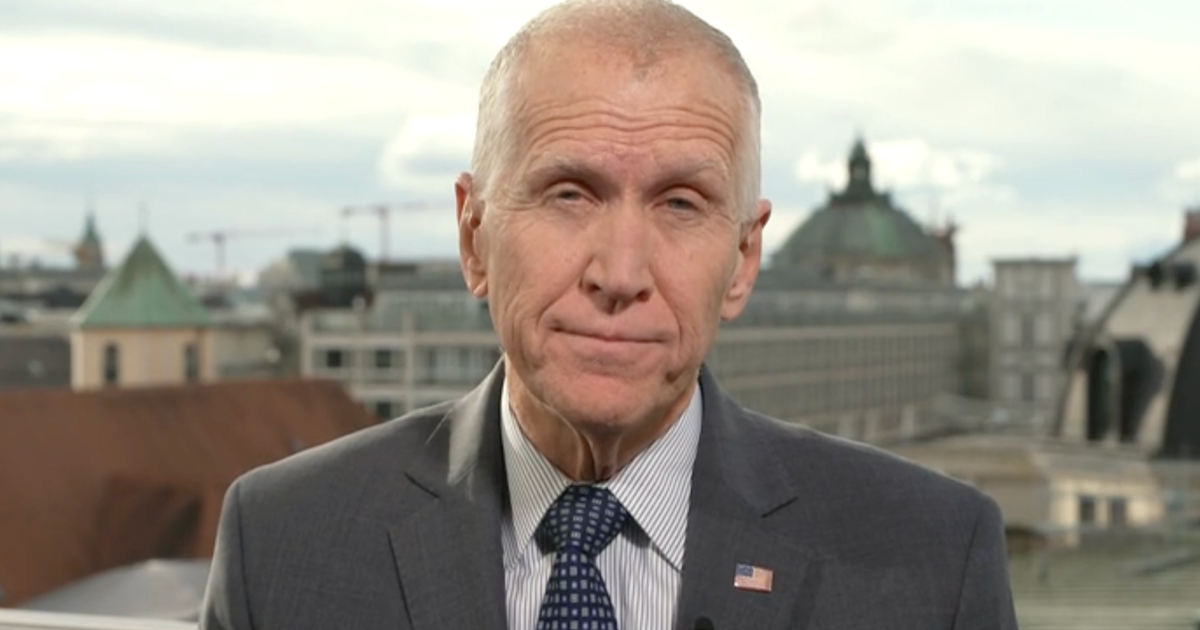
Transcript: Gianrico Farrugia on "Face the Nation," March 29, 2020
The following is a transcript of an interview with Mayo Clinic CEO Gianrico Farrugia that aired Sunday, March 29, 2020, on "Face the Nation."
MARGARET BRENNAN: We now go to the president and CEO of the Mayo Clinic, Dr. Gianrico Farrugia. He joins us from their campus in Rochester, Minnesota. Good to have you with us, Doctor. You may have--
DR. GIANRICO FARRUGIA: Well, thank you for having me on the show.
MARGARET BRENNAN: You may have just heard the governor of Louisiana tell us that his state is about to run out of ventilators. It's the one thing he says that keeps him up at night. And by April 10th, he doesn't expect to have enough hospital beds to accommodate the sick. Is this going to be the story across this country at hospitals?
FARRUGIA: Yes, this is a critical element of our conversation and discussion as a nation. We have to focus on saving lives, and saving lives means that we have to be very diligent about it because there is no direct end in sight. And therefore we have to continue to learn and improve as there is the wave of surges happens across our country. We have to really be diligent about focusing on what we can do to prevent people from getting sick. And if they're sick, how can we prevent them from entering into an ICU? And then once they get into an ICU, how can we make sure that their stay is as brief as possible? Because if, for example, you can go from 10 days on a ventilator to five days on a ventilator, then you can double the number of available ventilators. And Mayo Clinic, together with many other organizations, is- is laser-focused on doing this, focusing on- on testing and focusing on novel therapies to be able to- to really flatten and bend the curve.
MARGARET BRENNAN: One of the therapies that's gotten a lot of attention is these antibody serums. Tell me what your thoughts are on how effective that can be.
FARRUGIA: So we know that in order to really handle this crisis, we have to take many different approaches. The best antivirus still remains washing your hands, and we have to remind people of that. Then there are the antivirals themselves that attack the virus themselves. Then there are agents that are effective at blocking the molecules that the virus causes our own cells to release. And that can prevent some of the damage we're seeing in the lungs and other organs, including the kidneys. And then there are these convalescent ser- or convalescent plasma. Where you take plasma from a person who has had the virus and has recovered and has now an antibody response to it. And take that and in general, you can treat four people from one person. And doing so, you can provoke a artificial- a given response that allows them to recover more quickly. This is based on other diseases. It is now being tried for the coronavirus, for COVID-19. And Mayo Clinic and other institutions are working very hard, collaborating with industry to make sure that we can have adequate supply to test if this is going to make a difference. And I'm hopeful that it will.
MARGARET BRENNAN: We've also heard from epidemiologists about the hope of contact tracing, basically figuring out who you've come in contact with in order to determine how at risk you are. How would something like that work in the United States?
FARRUGIA: So every country has a different threshold on- on privacy of information, on data. But certainly we as a country have plenty of technology to do better at tracing. We've been collaborating, for instance, with M.I.T. on an app called Safe Paths where you can opt-in and then within your network you- you know if somebody within that network tested positive or even has symptoms. Now, we're working with a company called nference in Boston at really becoming better on predicting hot spots, because currently we're predicting hot spots very close to or even a little too late from when they start to occur. And you have the ability to use artificial intelligence to real-time know when a test is positive, but also understand things like, okay, how many tests happened in the last 24, 48 hours because that's really important. How many people are being admitted? You can get a much better idea of where the next hot spot is and then move resources. And in the last couple of days we've tried that. We've done that within the state of Minnesota. And we believe that there are many of these innovations that are happening across the country that will help us improve the way we trace and the way we advise people to be able to one, avoid getting sick and once they get sick, to understand what we can do for their immediate contact. And that is one of the very important ways that we can flatten that curve and at the same time inform the public, because, as you know, fear is a big part of this current pandemic.
MARGARET BRENNAN: Well- well based then on what you have seen so far, do you think that it is underestimated how much of this virus has already infected parts of the American Midwest?
FARRUGIA: There has been a lot of discussion about that. We have to be driven by the science, not by conjecture. I mean, we always have to be driven by the science. And to be driven by science, we need to have the right testing. And- and testing serology is gonna be very important that way to understand who has an antibody and therefore can be presumed to have had contact with the virus and has mounted a response to it. We at Mayo Clinic have spent a lot of time developing a first- a PCR test, now a serology test. There are many other institutions that are doing so, and this is where innovation and collaboration comes together because there is no one single test that is the right test. And there are many different tests that can be used. Serology for what you- for what you stated, but also trying to bring the price down. For example, the atomic agency in Austria is trying to use isotopes to develop a very cheap test.--
MARGARET BRENNAN: OK. Alright.
FARRUGIA: --the University of Washington, UC Berkeley are using CRISPR to try a different test as well as in New York--
MARGARET BRENNAN: Well- well thank you, doctor--
FARRUGIA: So what we're going to be seeing is a multitude of tests,--
MARGARET BRENNAN: OK.
FARRUGIA: --and that multitude of tests is going to be able to give us that- the answer to that question.
MARGARET BRENNAN: We wish you good luck. Thank you very much, Doctor.
FARRUGIA: Well, thank you very much.
MARGARET BRENNAN: We'll be right back.
FARRUGIA: And I really do want to thank every health care worker. Thank you.
MARGARET BRENNAN: We do, too.