Debunking tripledemic misconceptions with an Illinois immunologist
CHICAGO (CBS) -- March 2023 will mark three years since health officials declared COVID-19 a pandemic.
Now, high case numbers of both flu and RSV are in the mix, creating what some people are calling a "tripledemic."
Because misinformation can spread so quickly on social media, we sat down with an expert to debunk some common misconceptions about this "tripledemic." Dr. Jessica Brinkworth is an immunologist and assistant professor at the University of Illinois at Urbana-Champaign.
Immunity debt
One of those concepts is immunity debt. This idea was first used in an editorial opinion piece first in May 2021. The term has been used to describe the idea that COVID-19 mitigations such as the lockdown period in 2020 in the U.S. as well as masking and social distancing weakened people's immune systems. Therefore, now, there are more cases of COVID-19, RSV and flu.
Dr. Brinkworth says this term cannot be applied to the situation that we are in.
"There is a bunch of reasons to not apply immunity debt to this particular situation, the first one being that RSV doesn't trigger any longstanding immunity of any kind," she said, "and so for that reason alone, because the concept of immunity that relies on this notion of immune memory, it doesn't apply."
The second reason is that immunity debt does not consider vaccines.
"There's a long, nice body of work that demonstrates that the more influenza vaccines you have over the course of your lifetime for whatever strains are available, the more likely you are to be able to fend off incoming influenza," Brinkworth said, "and influenza immunity generally lasts quite a long time."
So then, why are there more cases of respiratory viruses? The answer is really complex, Dr. Brinkworth says.
Higher case numbers at unexpected times
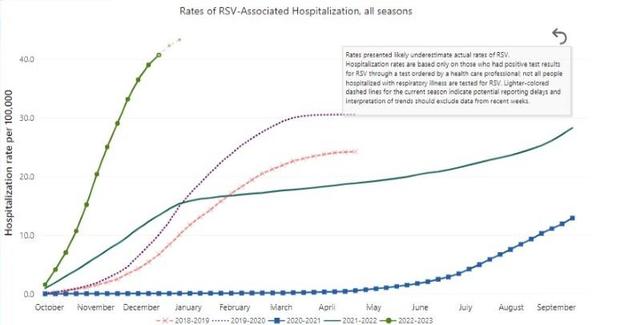
Part of the answer is that RSV has been on the rise for years, even before the pandemic. In 2019, there were 100,000 deaths in children under the age of 5 in RSV from RSV worldwide, according to data from the CDC.
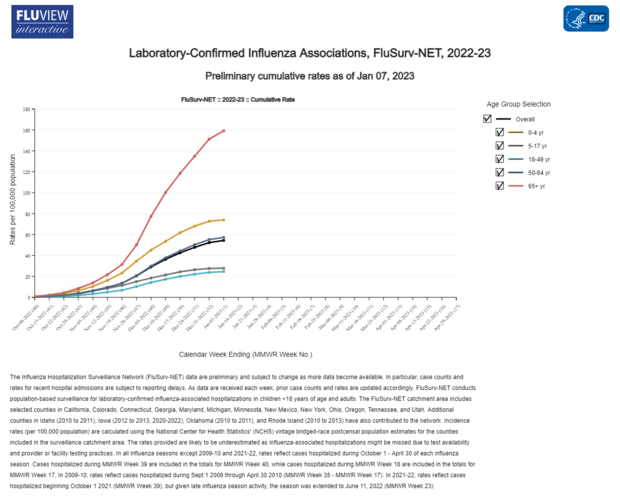
This year, both RSV and flu cases are much higher and peaked at unexpected times.
"Whenever we see shifts in flu patterns, we tend to see shifts in other seasonal pathogens," Brinkworth said.
Early flu hospitalizations hit a decade high in 2022. According to Centers for Disease Control and Prevention data, the last time was in 2009 with the H1N1 pandemic.
Between 2016 and 2020, RSV and Flu seasons substantially began to overlap. Then in the summer of 2021 with the lifting of COVID-19 restrictions, the flu season pushed far ahead.
Although we have some data on how RSV and flu interact, we are still learning more about how COVID-19 interacts with these two viruses.
Health experts do know that co-infections do occur and having one virus makes someone more susceptible to contracting other viruses. This increases the chances of mortality, says Brinkworth.
There is new research from the CDC that found that children under 5 who were hospitalized with COVID, and tested positive for a second virus, are more likely to be admitted to the ICU.
RSV
Another common misconception about the tripledemic, Brinkworth tells us, is that RSV only impacts children.
"One of the things that I think has been missed in the story of RSV this year is that also it is an important pathogen for at-risk adults. So that includes frail and elderly people; people who are immunocompromised," she said. About 78 percent of RSV-related deaths are among people 65 years and older. "It's been said to cause this really big disease burden that's at least as comparable to diseases like influenza,' Brinkworth said.
RSV's incubation period, or the time between getting infected and showing symptoms, is four days. There is also evidence that shows that contracting RSV doesn't give the immune system much immunity, or memory on how to protect against reinfection.
XBB.1.5
XBB.1.5 is the official name for the latest COVID-19 variant. It was first detected in the U.S. in October 2022, and as of Jan. 14, it already accounts for over 40 percent of U.S. cases.
"The Kraken" has caught on as a nickname for XBB1.5, and Brinkworth says, "It's a good representation of how fearful experts are that it's going to cause a lot of damage."
XBB1.5. Is a combination of other Omicron variants. It is the most transmissible variant of concern to date and is better at getting into cells.
A Washington-based lab that studies the evolution of viruses predicted this strain around a year ago.
"Bloom Lab looked at the sequences of available strains at the time and said that, 'Here are
the amino acids that I would change in these protein sequences, given what I know the function is if I wanted to be unbeatable," Brinkworth said.
Protection
Although there are no longer widespread mitigations enacted, Dr. Brinkworth emphasizes they are the best way to protect yourself and others.
"My strongest suggestion is always to mask and limit indoor closed time with large groups of people," she said.
The latest COVID-19 booster specifically targets Omicron strains. Receiving vaccinations against COVID-19 and influenza helps protect against severe illness and death.